The word ‘depression’ is often used colloquially, so you might hear someone saying ‘I felt so depressed after that argument’ and often what they mean is that they felt sad or fed up. Depression in the clinical sense is more than feeling sad in response to something. Clinical depression is really a cluster of symptoms including feeling sad or feeling low or flat; as well as feeling physically and emotionally drained or lethargic, losing interest and motivation in activities or relationships including those that used to bring us an enormous sense of fulfillment and pleasure; and other symptoms. Additionally, these symptoms are typically experienced consistently over a period of weeks, months or years. Now, it’s important to note that even if you have clinical depression, you might not feel depressed everyday, there might be some days or situations where you feel a little bit better; likewise, many people with depression hide it from the rest of the world for a very long time so on the surface may be the life of the party and may be able to joke and laugh with us, but are experiencing their own sense of internal suffering throughout.
There are number of factors that can cause depression, having others in our family with psychological disorders can make us more susceptible; having a ‘personality where you tend to be more self-critical or pessimistic (NOTE: life experiences typically also cause critical or pessimistic thinking rather than this being biologically determined). Significant life events can also cause depression, such as illnesses, losses or increased stress. Thinking specifically about COVID-19, all of the factors I’ve just mentioned are ones which many people might have experienced and may cause some people to experience some symptoms of depression.
The thing with depression is that it typically causes a range of changes, these might include, wanting to sleep all the time (or not wanting to sleep at all); not wanting to do the things we used to enjoy, or wanting to withdraw from loved ones and isolate ourselves. Importantly, it can also cause what’s called cognitive biases. A cognitive bias is a sort of ‘thinking error’ that can impact the way that we process and interpret events and experiences around us. In the case of depression, it can cause us to focus on/notice and interpret things in a more critical or negative light. Now these things might be caused by depression but they can also contribute towards and maintain our depression so we can end up in a sort of endless, vicious cycle.
When I’m working with people experiencing these symptoms, one of the strategies that we work on developing, is what’s called an ‘act opposite’ strategy. Act opposite is a technique that can be found in dialectical behaviour therapy (DBT) but in applying it to working with people with depression, the aim is to help identify the things that depression specifically is causing them to do that might actually be maintaining their depression and to figure out the ways in which they might act opposite to responses. Here are some examples:
1. Wanting to withdraw and isolate from friends and family?
Act opposite by calling a friend for a 5 minute chat (longer if you can manage), try to do this consistently and gradually increase your contact.
2. Wanting to sleep all day?
Act opposite by setting an alarm and maybe an additional one in another part of your room/house so that it forces you to get up to turn it off. Then take the day one step at a time, have a shower, have some breakfast etc. it can help to have a routine or plan already written down about what you might do that day.
3. Thinking very critically or negatively about everything?
Act opposite by writing down 1 thing that you feel grateful for each day. This can be ‘simple’ things like, ‘having running water so I could take a shower’. Try to write a different thing each day instead of writing down the same thing repeatedly, and try to write something that falls into different categories, for example, 1 thing you’re grateful for about the weather, 1 about your physical safety, 1 thing about your physiological needs being met, 1 thing about your social needs being met and so on.
Disclaimer: The information provided is advisory but should not replace any further specialist mental health or medical input, should you need this.
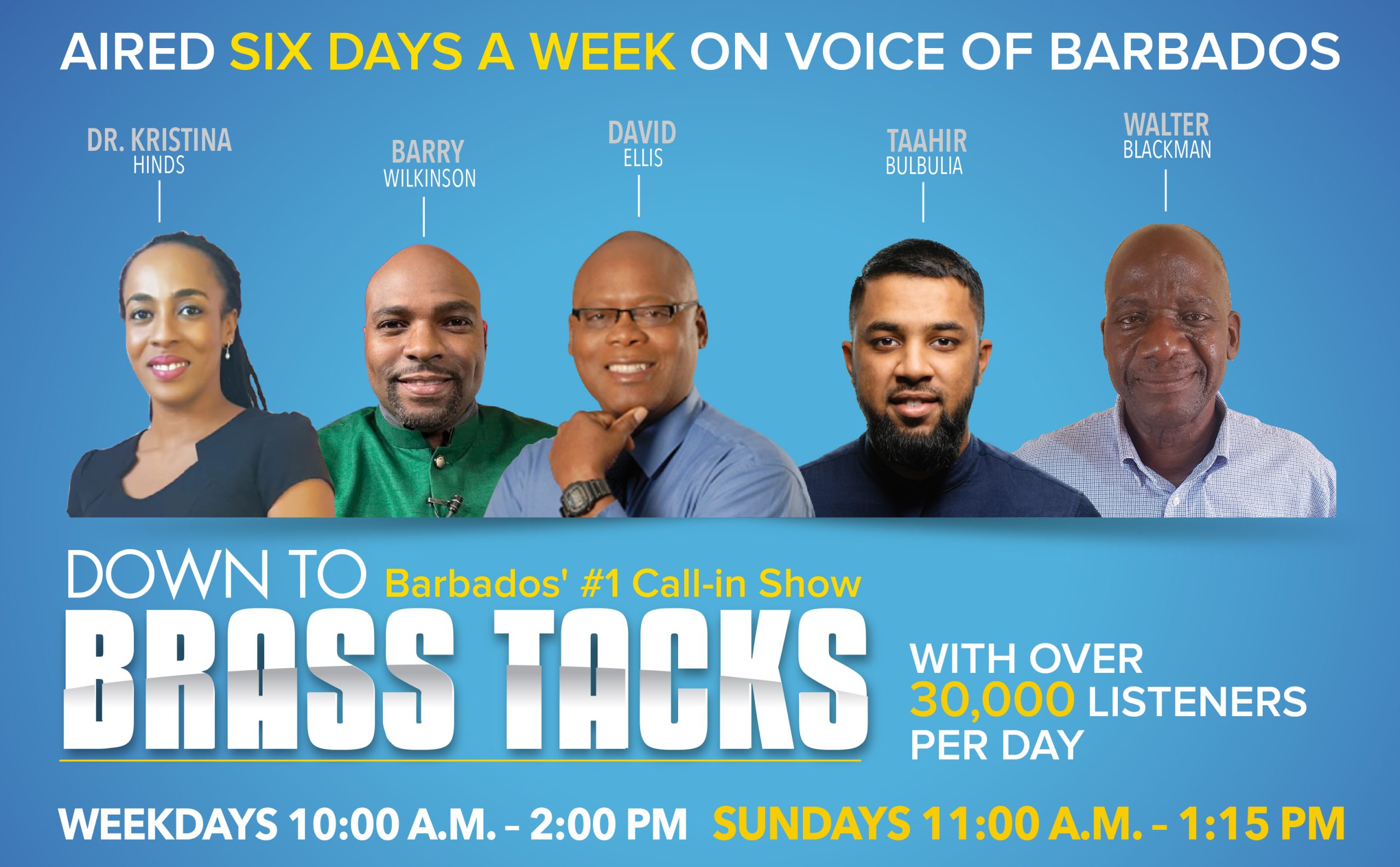
How To Manage Feelings of Depression During and Post Lockdown? by Chartered Counselling Psychologist Dr Tamara Vaughan of Mind Health Psychology